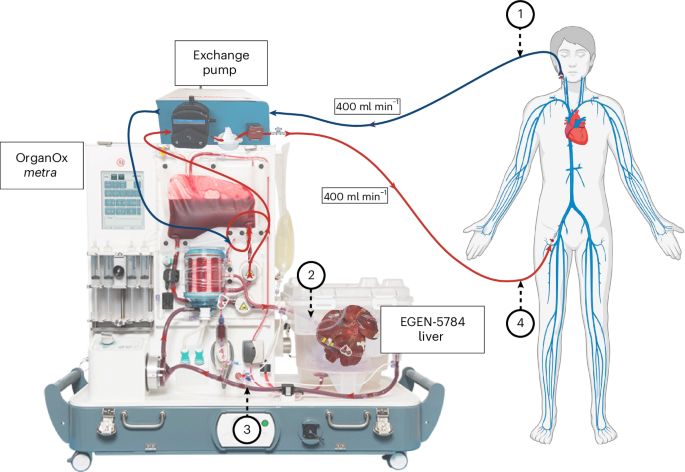
Extracorporeal cross-circulation with genetically modified pig livers in a human decedent model
Key Takeaway:
Researchers successfully used genetically modified pig livers to temporarily support human liver function, offering a potential new approach for liver failure treatment in the future.
For Clinicians:
"Pilot study (n=1). Demonstrated feasibility of extracorporeal pig liver support with minimal immunosuppression. No immediate clinical application; further research needed on safety, efficacy, and immunological impact before considering clinical use."
For Everyone Else:
This is early research on using pig livers for temporary support. It's not available in clinics yet. Continue following your doctor's advice and don't change your care based on this study.
Citation:
Nature Medicine - AI Section, 2026. Read article →