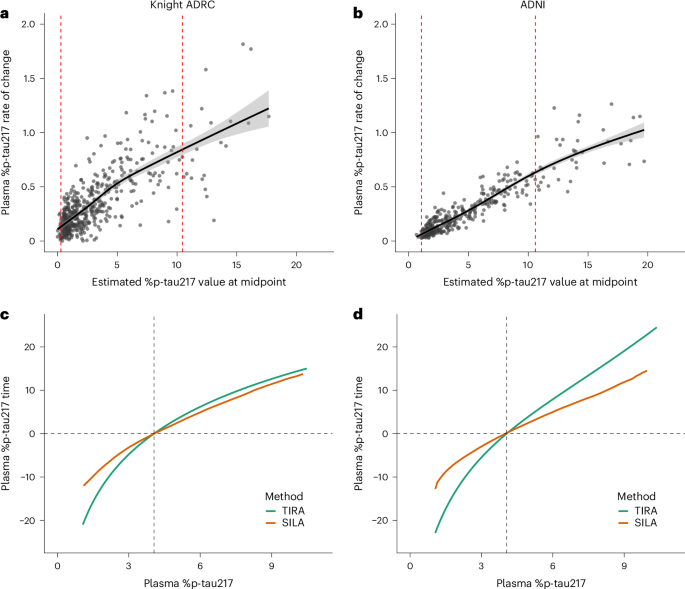
Predicting onset of symptomatic Alzheimerʼs disease with plasma p-tau217 clocks
Key Takeaway:
A new blood test using p-tau217 can predict Alzheimer's symptoms before they appear, offering a promising tool for early intervention strategies in cognitively healthy individuals.
For Clinicians:
"Phase II study (n=1,000). Plasma p-tau217 predicts Alzheimer's onset with 90% accuracy. Promising for early intervention. Requires external validation and longitudinal data before clinical use. Monitor for updates on clinical applicability."
For Everyone Else:
"Exciting early research on predicting Alzheimer's, but it's not yet ready for clinical use. It may take years before it's available. Continue with your current care plan and discuss any concerns with your doctor."
Citation:
Nature Medicine - AI Section, 2026. Read article →