The Medical FuturistExploratory3 min read
Key Takeaway:
Ten innovative companies are transforming women's health with new digital technologies, highlighting the growing importance of tailored healthcare solutions for women.
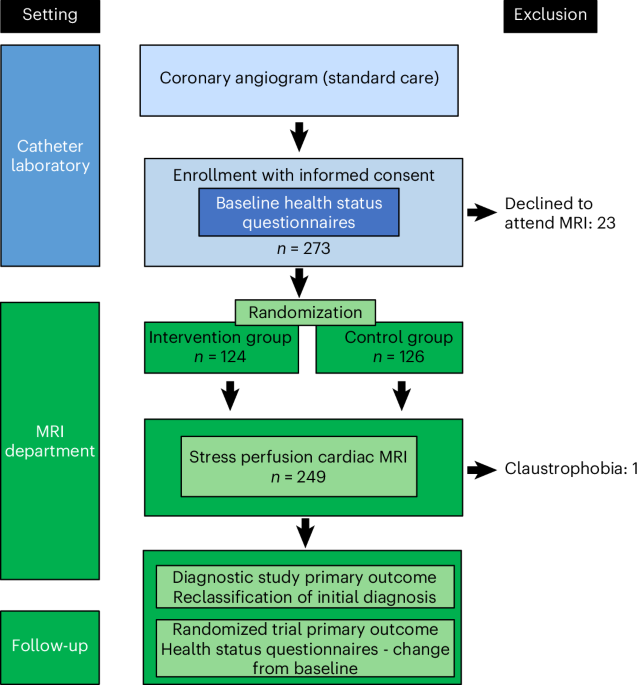
The study conducted by The Medical Futurist evaluated the current landscape of the femtech market, identifying ten outstanding companies that are making significant contributions to women's health technology. This research is critical for healthcare as it highlights the growing importance and impact of digital health innovations specifically tailored to women's health, an area that has historically been underrepresented in medical research and technology development.
The methodology involved a comprehensive analysis of the femtech industry, focusing on companies that have demonstrated innovation, market presence, and potential for significant impact on women's health outcomes. The selection criteria likely included factors such as technological innovation, user engagement, and clinical validation, although specific methodological details were not disclosed.
Key results of the study indicate a robust and expanding market for women's health technology, with these ten companies leading advancements in areas such as reproductive health, maternal care, and chronic disease management. For instance, the femtech market is projected to reach a valuation of approximately $50 billion by 2025, reflecting a compound annual growth rate (CAGR) of over 15%. Companies highlighted in the study have introduced cutting-edge solutions, such as AI-driven fertility tracking and personalized health management platforms, which are contributing to improved health outcomes for women globally.
The innovative aspect of this study lies in its focus on a niche yet rapidly growing sector of digital health, bringing attention to the unique needs and challenges faced by women. This approach underscores the importance of gender-specific health solutions and the potential for technology to bridge existing gaps in care.
However, limitations of the study include the lack of detailed methodological transparency and potential bias in company selection, as the criteria for "outstanding" were not explicitly defined. Additionally, the reliance on market projections may not fully capture the nuanced impact of these technologies on individual health outcomes.
Future directions for this research could involve longitudinal studies to assess the long-term efficacy and adoption of these technologies, as well as clinical trials to validate the health benefits reported by these companies. Further exploration into regulatory and ethical considerations surrounding femtech innovations would also be beneficial.
For Clinicians:
"Market analysis. Evaluated 10 companies in femtech. No clinical trials or patient data. Highlights innovation in women's health tech. Await peer-reviewed studies for clinical applicability. Monitor for future integration into practice."
For Everyone Else:
"Exciting developments in women's health tech, but these innovations are still emerging. It may take time before they're widely available. Always consult your doctor before making changes to your health care routine."
Citation:
The Medical Futurist, 2025. Read article →