MIT Technology Review - AIExploratory3 min read
Key Takeaway:
Most companies, including those in healthcare, struggle to move AI projects beyond testing stages despite significant investments, highlighting a need for better integration strategies.
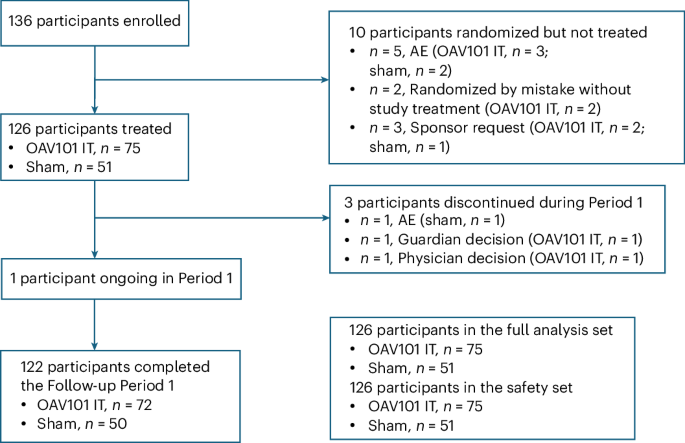
The study, published by MIT Technology Review - AI, investigates the dynamics of human-AI collaboration in developing an AI roadmap that effectively transitions from pilot projects to full-scale production, revealing that three-quarters of enterprises remain entrenched in the experimental phase despite substantial AI investments. This research holds significant implications for the healthcare sector, where AI technologies have the potential to revolutionize diagnostics, treatment personalization, and operational efficiencies. However, the transition from pilot studies to practical applications in clinical settings continues to present a formidable challenge.
The study employed a qualitative analysis of corporate AI initiatives, examining the strategic frameworks and operational challenges faced by organizations attempting to integrate AI systems beyond preliminary trials. Data was gathered through case studies and interviews with key stakeholders across various industries, including healthcare, to elucidate common barriers and successful strategies.
Key findings indicate that while investment in AI technologies has reached unprecedented levels, with a substantial portion of organizations allocating significant resources towards AI development, 75% remain in the experimental phase without achieving full production deployment. The study highlights that the primary barriers include a lack of strategic alignment, insufficient infrastructure, and the complexities of integrating AI systems into existing workflows. Furthermore, the research underscores the importance of fostering human-AI collaboration to enhance decision-making processes and improve AI system efficacy.
The innovative aspect of this research lies in its comprehensive approach to understanding the multifaceted challenges of AI deployment, emphasizing the necessity of human-AI synergy as a critical component for successful implementation. However, the study is limited by its reliance on qualitative data, which may not fully capture the quantitative metrics necessary for assessing AI deployment success across different sectors.
Future directions for this research include conducting longitudinal studies to evaluate the long-term impact of human-AI collaboration on AI deployment success rates and exploring sector-specific strategies for overcoming integration challenges, particularly in the healthcare industry.
For Clinicians:
"Qualitative study (n=varied enterprises). Highlights 75% stuck in AI pilots. Limited healthcare-specific data. Caution: Ensure robust validation before integrating AI tools into clinical workflows. Await sector-specific guidelines for full-scale implementation."
For Everyone Else:
This research is in early stages and not yet in healthcare settings. It may take years to see results. Continue with your current care plan and consult your doctor for personalized advice.
Citation:
MIT Technology Review - AI, 2025. Read article →