Nature Medicine - AI Section⭐Exploratory3 min read
Key Takeaway:
Psychedelic medicine shows promise in treating mental health disorders, offering new therapeutic options as research continues to grow in this field.
The review article published in Nature Medicine examines the scientific underpinnings of psychedelic medicine, providing a comprehensive synthesis of mechanistic insights and clinical evidence related to its use in treating neuropsychiatric disorders. This research is pivotal in the context of healthcare as it addresses the growing interest in alternative therapeutic approaches for conditions such as depression, anxiety, and PTSD, where conventional treatments may have limited efficacy or undesirable side effects.
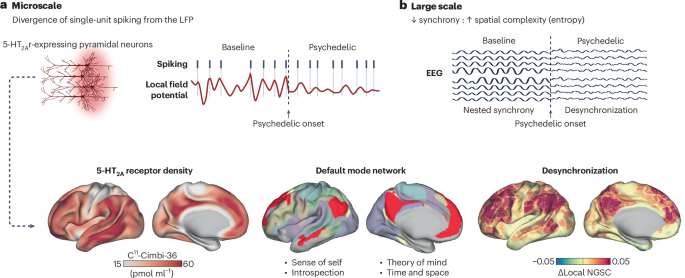
The review integrates data from various preclinical and clinical studies, employing a multidisciplinary approach that includes neuroimaging, pharmacology, and psychological assessments. By analyzing both the biochemical pathways affected by psychedelics and their clinical outcomes, the authors aim to elucidate the therapeutic potential and limitations of these substances.
Key findings from the review highlight that psychedelics, such as psilocybin and LSD, demonstrate significant efficacy in reducing symptoms of depression and anxiety, with response rates ranging from 60% to 80% in controlled trials. Neuroimaging studies reveal that these substances facilitate increased connectivity between brain networks, potentially underpinning their therapeutic effects. Furthermore, the review discusses the role of psychedelics in enhancing neuroplasticity, which may contribute to sustained symptom relief.
The innovation of this review lies in its integration of mechanistic and clinical perspectives, offering a holistic view of how psychedelics exert their effects at both molecular and systemic levels. However, the authors acknowledge limitations, including the small sample sizes and short duration of many clinical trials, which may affect the generalizability of the findings. Additionally, the potential for adverse psychological reactions necessitates careful consideration in clinical applications.
Future research directions proposed include larger-scale clinical trials to validate these findings, as well as investigations into the long-term effects and safety of repeated psychedelic use. The review underscores the need for rigorous scientific inquiry to fully harness the therapeutic potential of psychedelics in medicine.
For Clinicians:
- "Review of psychedelic medicine. Mechanistic insights and clinical evidence for neuropsychiatric disorders. No specific phase or sample size. Limited by early-stage research. Caution: Await further trials before clinical application."
For Everyone Else:
"Exciting early research on psychedelics for mental health, but not yet available in clinics. It may take years. Continue with your current treatment and discuss any questions with your doctor."
Citation:
Nature Medicine - AI Section, 2026. DOI: s41591-025-04194-5 Read article →